Decidual Cast
A decidual cast occurs when the uterine lining sheds all at once as a single, solid piece of tissue, instead of breaking apart gradually during a menstrual period. This intact sheet often takes on a triangular, uterus-shaped form, which can be alarming when passed through the vagina. Some clinicians refer to this event as membranous dysmenorrhea, and it may be associated with hormonal contraceptives, rapid progesterone shifts, or—less commonly—an ectopic pregnancy. Because the endometrial lining (decidua) detaches in one piece, many people experience sudden cramping, pelvic pain, or anxiety before the tissue is expelled.
In my clinical experience, seeing or passing a decidual cast is shocking, especially for someone who has never heard of it. But medically, it is usually benign, short-lived, and simply reflects the body’s response to hormonal changes. Understanding what the tissue looks like, why it forms, and how it differs from pregnancy-related events helps people recognize that although the process is uncomfortable, it rarely signals long-term reproductive problems.
Definition
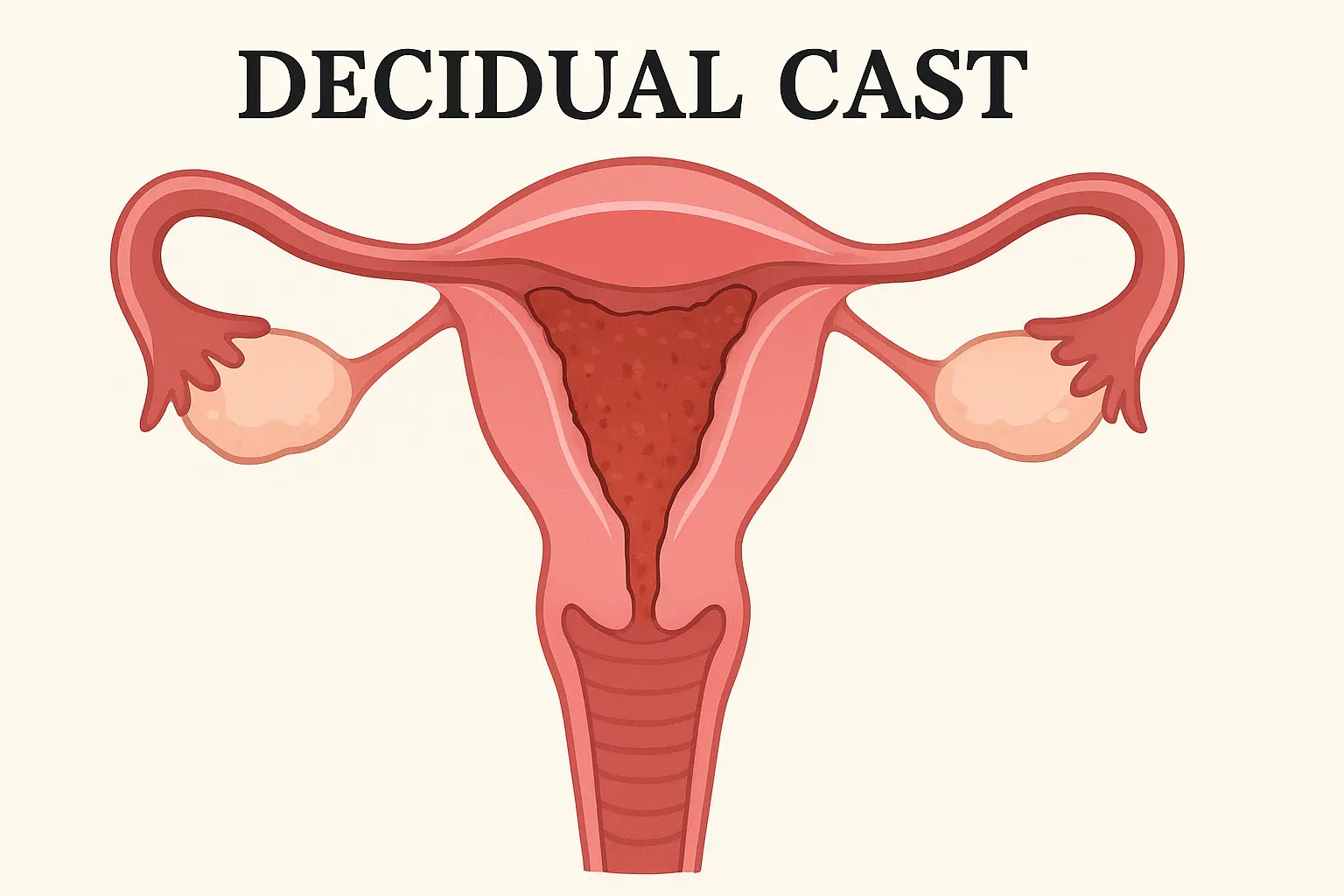
A decidual cast is the expulsion of the uterine lining in one complete piece, often retaining the shape of the uterine cavity. The name comes from the Latin deciduus, meaning “to fall off,” referring to the natural shedding of the endometrium. Normally, the lining breaks down and leaves the uterus in small fragments during a menstrual period. In rare situations, however, the tissue stays intact and exits as a single structure through the vaginal canal. This gives it a distinctive appearance—sometimes fleshy, sometimes triangular—that often triggers confusion or fear.
Social media platforms, especially TikTok, have recently amplified stories of decidual casts, sometimes mixing credible information with exaggerated claims. Understanding the biology behind the event helps people approach it with clarity rather than panic.
What is a decidual cast?
A decidual cast occurs when the thickened decidual lining sheds suddenly and exits the uterus as one large, structured piece. It often mimics the internal shape of the uterus, leading to a triangular or cone-like cast. While the appearance may suggest something serious, in most cases it is a temporary response to hormonal imbalance, contraceptive changes, or rarely, early pregnancy complications. Cramping, bleeding, and discomfort are common, but with appropriate evaluation by an OBGYN, most people recover quickly.
Is a decidual cast bad?
A decidual cast can be painful and emotionally distressing, but it is not inherently dangerous. The tissue may look unusual, but it typically reflects a short-term hormonal fluctuation rather than a serious medical condition. Throughout history, medical literature has consistently described decidual casts as rare but benign events.
Still, because severe cramping or tissue passage can resemble symptoms of pregnancy loss or ectopic pregnancy, professional evaluation is often recommended to provide reassurance.
How common is a decidual cast?
Decidual casts are rare, and many clinicians may see only a handful of cases in their entire careers. Despite occasional viral moments online, the event itself is uncommon and usually occurs only once in a person’s lifetime.
Symptoms and Causes
What are the symptoms of a decidual cast?
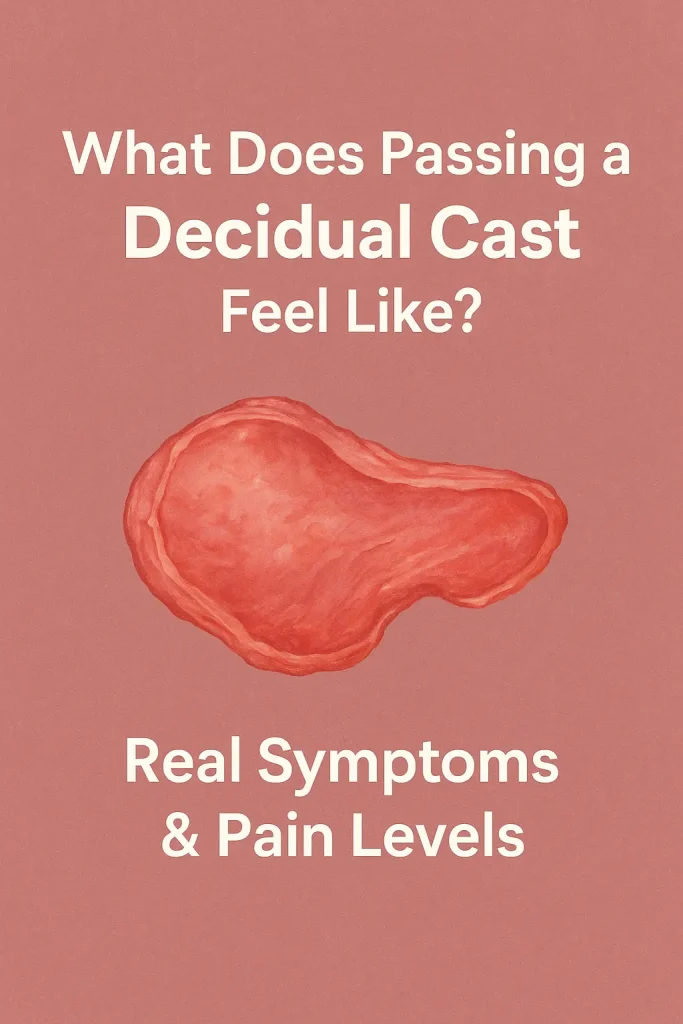
A decidual cast is often preceded by sharp, intense cramping as the firm tissue moves through the cervix. Symptoms can include:
- Severe menstrual-like cramps
- Pelvic or lower abdominal pain
- Vaginal bleeding or spotting
- Nausea, dizziness, or faintness
- Heavy bleeding immediately before or after expulsion
The expelled tissue is typically pink, red, or gray, with a fleshy, rubbery consistency. It may measure 1–4 inches and often maintains a triangular or light-bulb shape that resembles the uterine cavity.
The experience is startling, but symptoms usually resolve within a day. Bleeding may continue for several days afterward.
What does a decidual cast look like?
A decidual cast often:
- Appears red, pink, gray, or whitish
- Has a fleshy, skin-like texture
- Retains the triangular or pear-shaped outline of the uterus
- May feel firm, rubbery, or membranous
Some individuals describe it as resembling a large clot, but unlike clots, a decidual cast holds its shape. Medical literature notes that a typical adult uterus measures roughly 3 inches long and 2 inches wide, which explains why casts can appear surprisingly large.
How big is a decidual cast?
In confirmed cases, many people describe the tissue as larger than expected—often about the size of a palm, a walnut, or even a small lime. Size varies depending on how thick the lining became before detaching. Everyday comparisons help reduce panic when someone first encounters the cast, especially since its structured appearance often comes as a shock.
Can a decidual cast come out in pieces?
Yes. While some people pass the tissue intact, others shed it in pieces, especially if the lining detaches unevenly. It may be:
- Fragmented
- Partial
- Released as smaller sections
- Sloughed off gradually
- Expelled as a firm clump of tissue
All these patterns fall within the normal range. The shape simply depends on how the lining separated during the menstrual cycle or after early pregnancy-related hormonal shifts.
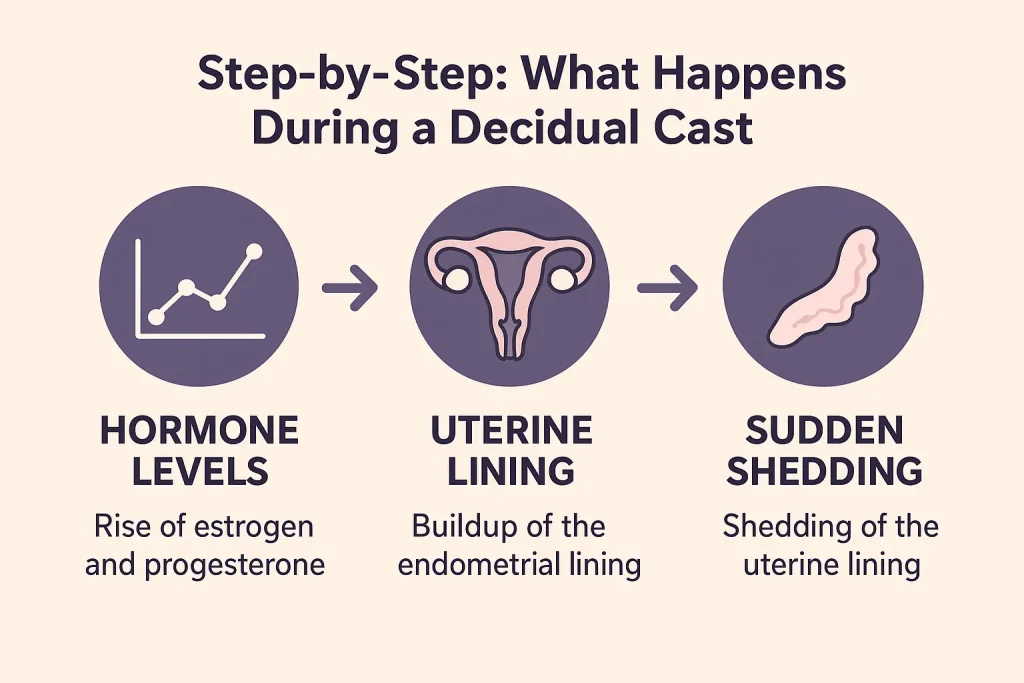
What causes a decidual cast?
A decidual cast forms when the uterine lining becomes unusually thick or structured—often due to progesterone imbalance—and then sheds suddenly as a single unit. Common causes include:
1. Hormonal contraceptives (birth control)
Changes in pills, injections, implants, or emergency contraception can cause the lining to solidify, making it more likely to detach in one piece.
2. Ectopic pregnancy
Although uncommon, an ectopic pregnancy can trigger unusual shedding of the lining. This is a medical emergency, so immediate evaluation is essential when symptoms overlap.
3. Hormonal changes
Natural fluctuations during the menstrual cycle or following early pregnancy can cause the endometrium to detach intact rather than in fragments.
4. COVID-19 vaccination
A small number of individuals have reported temporary menstrual changes after vaccination, including rare decidual-like tissue shedding. Current evidence suggests these effects are short-term and not harmful.
What makes you more likely to have a decidual cast?
Factors that increase the likelihood include:
- Hormonal contraceptives
- Emergency contraception
- IUD use
- Irregular ovulation
- Past ectopic pregnancy
- Sudden progesterone shifts
Most people who experience a decidual cast never have another one.
What are the complications of a decidual cast?
omplications are rare. The main concerns include:
- Severe cramps during passage
- Heavy vaginal bleeding
- Temporary inflammation
- Confusion with miscarriage or ectopic pregnancy
Once expelled, the tissue usually causes no ongoing problems.
Is a decidual cast a miscarriage?
No. A decidual cast is not a miscarriage. It contains uterine lining only, not fetal tissue.
However, because symptoms overlap, healthcare providers may check a pregnancy test to rule out pregnancy-related conditions.
Diagnosis and Tests
How do you know if it’s a decidual cast?
Most people recognize a decidual cast by its distinct shape. The tissue often looks like a molded outline of the uterus and is firmer than a typical clot. Sharp cramps before expulsion are also a clue.
A pregnancy test can help distinguish it from miscarriage.
Can a decidual cast be diagnosed?
Diagnosis is mainly based on visual examination of the tissue. Imaging is usually not required unless symptoms suggest an ectopic pregnancy or other complication. Providers often ask about hormonal medication, contraceptive use, and recent cycle changes to confirm the cause.
Why do decidual casts happen?
Decidual casts occur when progesterone levels rise and fall abruptly, causing the uterine lining to thicken and then shed all at once. This process explains why they are occasionally associated with contraceptive changes, stress, early pregnancy, or irregular cycles.
Management and Treatment
How are decidual casts treated?
Once the tissue passes, treatment focuses on symptom relief:
- Heating pads
- NSAIDs (ibuprofen, naproxen)
- Rest and hydration
Because the cast is already expelled, no procedure is typically required.
Risks of a decidual cast
Risks are minimal, but medical attention is essential if symptoms include:
- Signs of ectopic pregnancy
- Persistent heavy bleeding
- Severe, worsening pelvic pain
- Dizziness or faintness
Natural Remedies and Lifestyle Changes
When I’ve spoken to women who went through this, many found comfort with gentle remedies: warm compresses on the lower abdomen, hydration, magnesium-rich foods, and rest.
Creating hormonal stability also helps—regular sleep, stress management, and avoiding sudden changes in hormonal contraceptives unless supervised.
Outlook / Prognosis
Can a decidual cast cause infertility?
No. A decidual cast does not affect fertility. Once the lining rebuilds normally, the uterus functions just as it did before. I’ve seen women conceive naturally even a month or two after experiencing one.
What can I expect if I pass a decidual cast?
Most people feel intense cramping during passage, followed by quick relief. Bleeding afterward resembles a menstrual period. Emotionally, the experience may feel unsettling, but physical recovery is usually fast.
Is passing a decidual cast routine?
No—decidual casts are rare. Most people will never experience one.
Prevention
Can you prevent a decidual cast?
Complete prevention isn’t possible, but maintaining stable hormonal patterns—consistent pill timing, supervised contraceptive changes, and regular monitoring if using an IUD—can reduce the likelihood.
Living With
When should I see my healthcare provider?
Seek help if you aren’t sure what you passed, if pain is unbearable, if bleeding is heavy, or if there’s any chance of an ectopic pregnancy. A doctor’s reassurance alone can make a huge difference when the experience feels alarming.
Should You Be Worried?
A decidual cast looks dramatic, but it is rarely harmful. Concern is warranted only if symptoms persist or suggest pregnancy complications.
Tips for Managing the Discomfort
Many individuals benefit from:
- Hydration and electrolytes
- A heating pad
- Light walking
- Avoiding heavy exercise
Decidual cast and social media: analyzing the “trend”
Online platforms often amplify decidual cast stories, sometimes inaccurately linking them to miscarriage or severe disease. Misinformation spreads easily, causing unnecessary fear. Understanding the hormonal basis behind this rare event helps counter these misconceptions.
A note from Us
Medical specialists emphasize that while a decidual cast is dramatic and painful, it is generally benign. The primary medical concern is ruling out an ectopic pregnancy when symptoms overlap.
Summary
A decidual cast is a rare, intense form of endometrial shedding linked to hormonal imbalance, changes in progesterone, contraceptive use, IUDs, and occasionally early pregnancy. Although its appearance can resemble more serious conditions, proper evaluation ensures safety. Most people experience it only once, recover quickly, and maintain normal fertility.
